Conservative care
Conservative care or nonsurgical treatment involves a combination of medicine and splints. Some common treatments include:
- Icing the joint several times a day
- Taking anti-inflammatory (NSAIDs) medication
- Wearing a supporting splint
- Limiting movement or exercises
Since arthritis is a progressive condition, it may worsen over time and surgery may be required. If your condition is untreated and it progresses to stage IV (4) arthritis, some surgical treatments may not be available.
Surgical treatment
Since there is no way to replace cartilage, the goal of surgical treatment is to treat the condition by removing the bone-on-bone contact.
The most common surgical option and the treatment often presented to patients involves the complete removal of the trapezium bone at the base of the thumb, referred to as a trapeziectomy. First performed in 1973, a trapeziectomy has been the standard of care due to its effectiveness in relieving pain.1 There are several variations of the procedure, including LRTI and Suspensionplasty. While effective at reducing pain, these procedures involve a lengthy recovery, possible shortening of the thumb, and may reduce strength. Most importantly if unsuccessful, few options remain.
While not offered by all surgeons, many surgeons have turned to joint replacement instead, noting faster recovery, improved strength, and pain relief. Joint Replacement also preserves the trapezium bone, which gives the surgeon and the patient the option to perform an LRTI in the future if necessary.
Arthroscopy
The concept of arthroscopy may be most beneficial in the early stages of basal joint arthritis. During an arthroscopy, a small tube connected to a high-definition camera is inserted into the joint through a tiny incision. An arthroscopic evaluation of this joint gives a surgeon the true stage of arthritis. During arthroscopy, your surgeon may also remove bone spurs, perform an osteotomy to realign the joint or be able to make recommendations for another form of surgical correction.
Advantages
The procedure is low-risk and performed in a minimally invasive fashion. It allows the surgeon to assess the joint better than routine x-rays which may allow a quicker diagnosis of your condition.
Disadvantages
The procedure is mainly indicated in the early stages of arthritis and may not be beneficial if it has progressed to the late stages.
Trapeziectomy (Traditional Procedure)
It is reported that 90% of all surgeries to treat basal thumb arthritis involve the removal of the trapezium bone, which is called a trapeziectomy2. After removing the bone, most surgeries involve suspending the first metacarpal bone to the second metacarpal with either a suture or a tendon harvested from the forearm. This is done to help reduce the risk of the metacarpal bone moving into the space where the trapezium was and shortening the length of the thumb.
Trapeziectomy with LRTI (Ligament Reconstruction with Tendon Interposition)
The most common procedure performed is referred to as an LRTI, also called the anchovy procedure. During this procedure, a surgical incision is made in the forearm and the FCR (flexor carpi radialis) tendon is split. An incision is then made over the carpometacarpal (CMC) joint and the trapezium bone is removed. A hole is then drilled into the base of the metacarpal where the FCR is passed through, and the remaining tendon is rolled up into a coil and inserted into the empty space created by the removal of the trapezium bone.
After the procedure, you will be placed in a cast. The amount of time in a cast will vary depending on the surgeon and patient, however, it is often required for 8-12 weeks and replaced with a removable thumb spica splint. After 12 weeks, grip strengthening, and pinching exercises are begun.
Advantages
The LRTI has been the gold standard procedure that newer procedures are often compared to. The majority of studies find that it provides predictable pain relief since it removes bone-on-bone contact. Finally, due to its popularity, there are many surgeons experienced in the procedure allowing most patients the ability to be treated locally.
Disadvantages
The LRTI has several disadvantages such as lengthy recovery, thumb shortening (subsidence), and limited to no revision options. While pain relief is often expected, complication rates can be seen in up to one-third of cases.3,4 These complications can include symptomatic subsidence, pain, swelling, and wound healing. The biggest disadvantage is that there are few revision options, and studies show that revision LRTI patients reported significantly worse outcomes compared with primary patients.5
Trapeziectomy with Suspensionplasty
Another common procedure is called Suspensionplasty. This again involves removing the trapezium bone but instead of inserting a tendon into the joint, it is only suspended by either a suture or another tendon, typically the abductor pollicis longus (APL) tendon.
After the procedure, you will be placed in a cast. The amount of time in a cast will vary depending on the surgeon and patient, however, it is often required for 8-12 weeks and replaced with a removable thumb spica splint. After 12 weeks, grip strengthening, and pinching exercises are begun.
Advantages
The majority of studies find that it provides predictable pain relief since it removes bone-on-bone contact. If using a suture material to suspend the metacarpal, a tendon won’t need to be harvested. Finally, due to its popularity, there are many surgeons experienced in the procedure allowing most patients the ability to be treated locally.
Disadvantages
Suspensionplasty has the same disadvantages as an LRTI such as lengthy recovery, thumb shortening (subsidence), and limited to no revision options.
Joint Replacement (Implant Arthroplasty)
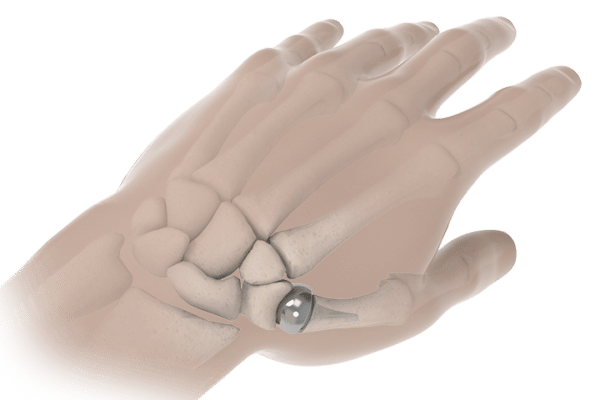
A joint replacement procedure involves removing the damaged cartilage and placing an artificial implant, similar to a hip replacement, in the joint to prevent bone-on-bone contact. There are two types of joint replacement, total joint replacement, and hemi joint replacement. A total joint replacement replaces both sides of the joint and requires a cup to be fixated into the trapezium bone and a stem into the metacarpal. A hemi joint replacement only replaces one side of the joint and will instead form a socket into the trapezium for the head to articulate into.
After the procedure, your hand is then placed in a cast for 2-4 weeks while your healing begins. After the cast is removed, grip strengthening and pinching exercises are begun. Most patients have unrestricted activity after 12 weeks.
Advantages
Joint replacement has many advantages including maintaining motion and a firm foundation for pinch and grip strength. Another significant advantage is that if joint replacement fails, a revision to a traditional procedure such as the LRTI is still available.6-7
Disadvantages
There are a variety of joint replacements available and not all have the same success rates. It is important to choose an implant with clinical data showing successful outcomes. There are not as many surgeons that perform joint replacement so receiving local treatment may be difficult.
- Turker T, Thirkannad S. Trapezio-metacarpal arthritis: The price of an opposable thumb! Indian J Plast Surg. 2011 May;44(2):308-16. doi: 10.4103/0970-0358.85352. PMID: 22022041; PMCID: PMC3193643.
- Yuan F, Aliu O, Chung KC, Mahmoudi E. Evidence-Based Practice in the Surgical Treatment of Thumb Carpometacarpal Joint Arthritis. J Hand Surg Am. 2017 Feb;42(2):104-112.e1. doi: 10.1016/j.jhsa.2016.11.029. PMID: 28160900; PMCID: PMC5302845.
- Gangopadhyay S, McKenna H, Burke FD, Davis TR. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012 Mar;37(3):411-7. doi: 10.1016/j.jhsa.2011.11.027. Epub 2012 Feb 3. PMID: 22305824.
- Naram A, Lyons K, Rothkopf DM, Calkins ER, Breen T, Jones M, Shufflebarger JV. Increased Complications in Trapeziectomy With Ligament Reconstruction and Tendon Interposition Compared With Trapeziectomy Alone. Hand (N Y). 2016 Mar;11(1):78-82. doi: 10.1177/1558944715617215. Epub 2016 Jan 14. PMID: 27418894; PMCID: PMC4920518.
- Sadhu A, Calfee RP, Guthrie A, Wall LB. Revision Ligament Reconstruction Tendon Interposition for Trapeziometacarpal Arthritis: A Case-Control Investigation. J Hand Surg Am. 2016 Dec;41(12):1114-1121. doi: 10.1016/j.jhsa.2016.09.005. Epub 2016 Oct 15. PMID: 27751779; PMCID: PMC5138108.
- Pritchett JW, Habryl LS. A promising thumb Basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res. 2012;470(10):2756-2763. doi:10.1007/s11999-012-2367-7
- Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am. 2008 Oct;33(8):1369-77. doi: 10.1016/j.jhsa.2008.04.028. PMID: 18929203.

